The elderly population is increasing globally including in developing countries like India. According to WHO, over the next 40 years, developing countries will have 80% of the world’s elderly population. Currently, elderly people comprise 8% of India’s population which is projected to rise to 19% by 2050. This increase in the number of elderly will present new challenges to healthcare. Since nutritional status is an important health predictor, and the elderly are particularly susceptible to malnutrition, it is extremely important to identify nutritional issues in the elderly and intervene accordingly.
Malnutrition in the elderly is associated with reduced mobility, compromised immunity, and cognitive impairment which reduce their overall functional ability.
What puts them at risk of malnutrition?
Malnutrition in elderly results from complex interplay of various factors-
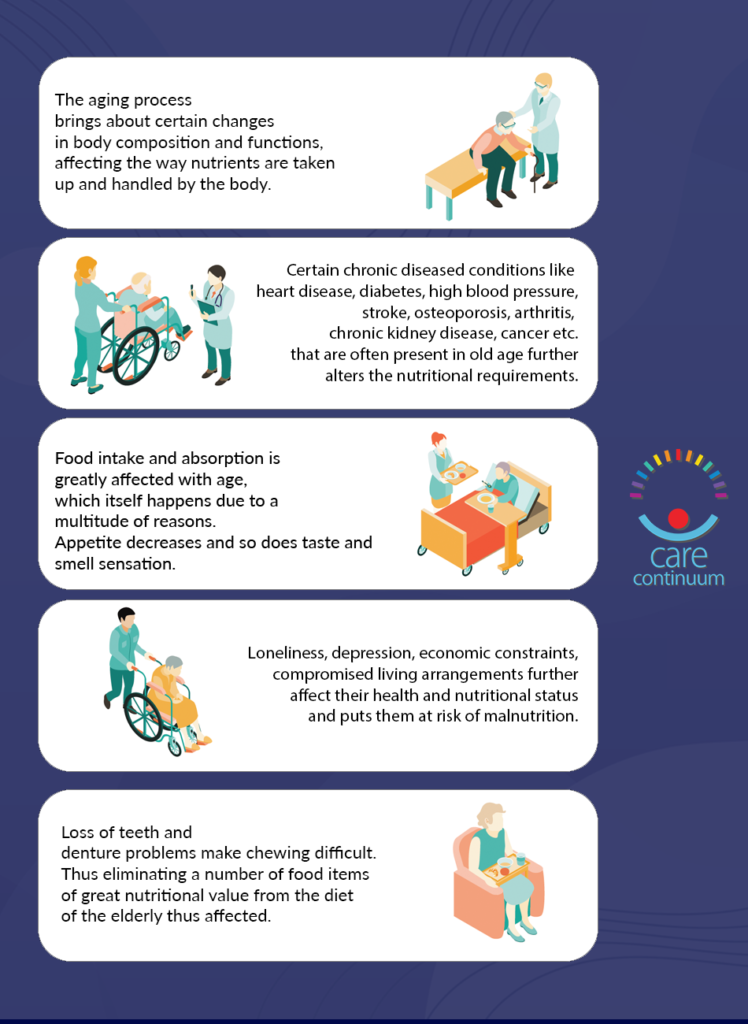
The aging process itself brings about certain changes in body composition and functions, affecting the way nutrients are taken up and handled by the body. This alters the requirement of some nutrients. With age, physical activity declines due to the decrease in the mass and strength of muscle and bones. The metabolic rate also decreases. Thus, elderly people have reduced caloric needs.
Secondly, certain chronic diseased conditions like heart disease, diabetes, high blood pressure, stroke, osteoporosis, arthritis, chronic kidney disease, cancer etc. that are often present in old age further alters the nutritional requirements. In fact, some of these conditions are caused in part due to inappropriate dietary habits and the presence of such conditions calls for dietary modifications.
Thirdly, food intake and absorption is greatly affected with age, which itself happens due to a multitude of reasons. Appetite decreases and so does taste and smell sensation. Loss of teeth and denture problems make chewing difficult. Acid reflux, constipation, frequent alternating episodes of diarrhea and constipation (irritable bowel syndrome), further hampers food intake. Food is no longer enjoyable and feeding often becomes a challenge especially if additional problems such as swallowing difficulties are present due to neurological causes. Chronic diseases often impose restrictions on certain food items which further reduces food intake. Nutrient absorption is also affected due to age related changes in the digestive tract. Thus, obtaining the desired nourishment becomes a challenge, which puts them at risk of developing malnutrition.
Lastly, loneliness, depression, economic constraints, compromised living arrangements further affect their health and nutritional status and puts them at risk of malnutrition.
Alongside malnutrition, another major concern in the elderly is dehydration, which is preventable. Aging brings about a decrease in thirst sensation which along with other factors like swallowing difficulties, multiple medications, altered mental status, and acute illnesses like diarrhea or vomiting put them at risk of dehydration.
Thus, nutritional intervention for elderly should aim at
- Preventing or delaying the development or progression of age-related chronic diseases.
- Identifying and correcting malnutrition
- Necessary modifications in diet as a part of disease management.
Nutrition advice for elderly-
It is difficult to give generalized advice. Dietary modifications might be required in terms of amount, quality, variety, and consistency. The first and foremost thing that should be kept in mind is that the diet should not be overly restrictive, especially for individuals with reduced appetite. It is more important to concentrate on overall diet quality and palatability.
E.g. if a person is supposed to be on a potassium restricted diet, instead of restricting all potassium-rich foods (such as fruits, pulses, leafy vegetables, etc) the total amount of potassium that person is currently consuming through his/her usual diet should be assessed and accordingly advised regarding the amounts of such food. It is often found that the overall food intake is so low that restriction is not required and might be detrimental.
Some generalized tips-
- Since the amount of food intake decreases, foods should be nutrient-dense, i.e., food preparations containing the maximum amount of nutrients per serving. Some examples are mixed veg khichdi, curd-chire-banana, oats porridge with dry fruits, and nuts.
- Foods should be well cooked, which are easy to chew, and gentle on the stomach.
- Include a wide variety of foods (unless otherwise indicated due to specific conditions) to ensure balanced nutrition.
- Foods should be well seasoned to enhance flavor and palatability especially for individuals who are on a restricted salt diet. Use of lime juice, herbs (curry leaves, coriander leaves, bay leaves, parsley, etc), and spices like jeera, mustard seeds improve flavour naturally and are better and safer than artificial seasonings.
- Many elderly individuals have inadequate protein intake due to digestibility issues, chewing problems, and various other factors. Adequate protein intake should be ensured in all individuals including those on a restricted protein diet. Foods like low-fat curd, chhena, fish, boiled eggs, masoor dals, are protein sources that are well tolerated.
- Adequate fibre intake should be ensured in the form of whole-grain foods (atta roti, brown bread, dalia, oats, muesli etc.), whole pulses, vegetables and fruits. Fibre ensures regular bowel movements, keeps the digestive system healthy, helps in lowering blood cholesterol and manages blood sugar. However, in certain individuals’ fibre is not well tolerated or might be contraindicated due to the presence of certain diseased conditions. In such cases, excess insoluble fibre (e.g leafy vegetables, beans, cabbage, whole pulses, whole wheat products etc.) should be avoided. However, foods like carrots, apple, oats, barley, banana, citrus fruits which are rich in soluble fibre should be included.
- Ensure adequate fluid intake in the form of plain water and liquid foods and beverages like vegetable soups, chicken broth, buttermilk, weak tea, coconut water, milk, etc. However, individuals with conditions like chronic kidney disease might require fluid and potassium restrictions. In such cases, plain water in specified amounts should be taken, and liquids like coconut water, vegetable soups, dal water should be avoided.